Various B scenarios
We will begin by looking at biological emergencies, which are also referred to as B scenarios. These are per se highly diverse.
A distinction is drawn between the following six types of scenario:
-
Single case of a disease involving highly pathogenic agents
-
Local epidemic
-
Supra-regional epidemic
-
Pandemic
-
Discovery of a suspicious substance/attack on individuals
-
Bioterrorist attack
Risk assessment
The term 'biological emergency' usually refers to the spread of infectious agents or corresponding toxins. To assess the risk in an acute situation it is helpful to identify the biological agent. A distinction needs to be drawn between whether the outbreak is taking place for instance in hospital, where the agent/hazard is usually known, or whether the situation involves an increased incidence of disease with similar presentations, the cause of which is unclear (both most closely resemble scenario 2 in the graphic 'Overview of different scenarios'). The latter would be conceivable for instance in a care home where there was an increased incidence of gastroenteritis symptoms. Another possibility here is the risk posed by 'bioterrorism' where the status in those affected is (still) unknown (comes closest to scenario 5 in the graphic 'Overview of different scenarios'). Here it is also crucial to have the right laboratory testing facilities available. Existing rapid tests are only partially reliable, particularly with environmental samples, and can produce both false positive and false negative results. To assess the risk it is therefore always necessary to have samples analysed in an experienced laboratory.
N.B.: Although the overwhelming majority of outbreaks have a natural cause, when assessing the risk the possibility of intentional release should always be considered.
Also include the following criteria:
-
Routes of infection
-
Treatment options
-
Available protective measures
-
Likelihood of spread
One option for performing a risk assessment prior to an emergency would be to produce a matrix of the extent of damage and likelihood of occurrence, for example.
A risk matrix can help assess the anticipated scope of damage, as shown in the graphic 'Overview of different scenarios' (source: Generic plan for biological emergencies – based on 5 scenarios; version 2.0 | Senate Department for Health and Social Services – graphic modified in scenarios 5 and 6).
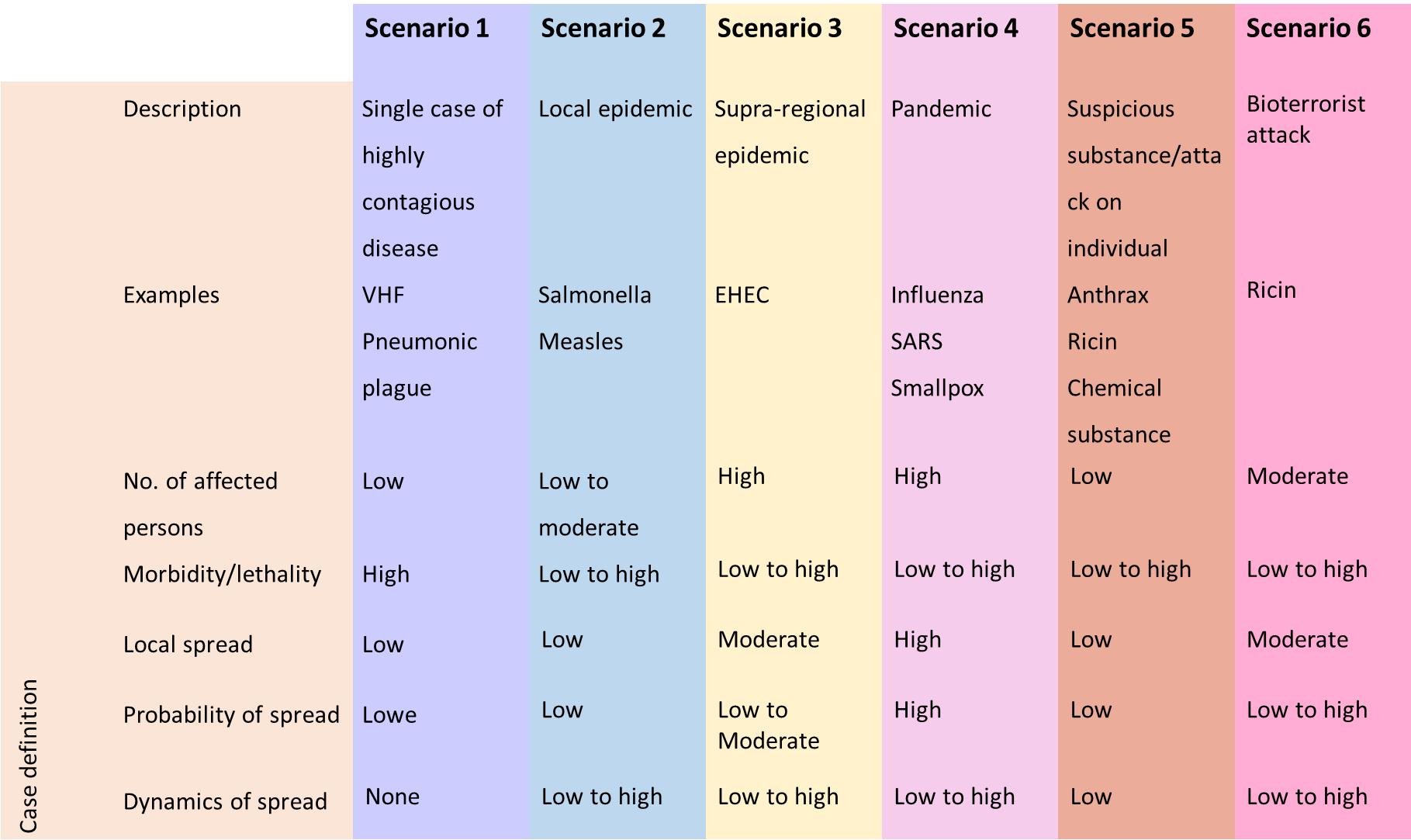
Figure 8: Overview of different scenarios
To assess the risk it is also necessary to define the objective that can be achieved in the respective situation. At the beginning of an epidemic, for example, the objective may be to prevent or at least delay the outbreak. Once an epidemic has taken hold, on the other hand, the focus may be on maintaining the life of society.
Measures
The transitions between the three phases described below are smooth, hence when assessing the risk it will be necessary to gradually adjust the measures employed. See the information published by the RKI in its Epidemiological Bulletin 7/2020 on Objectives of infection control measures.
Containment
In this phase an attempt is made to identify every infected person as soon as possible and isolate them immediately. All contacts are traced and placed under observation or where appropriate on the quarantine (especially with diseases where others can be infected before symptoms begin), in order to break the chain of infection as quickly as possible.
This strategy aims to eradicate the pathogen. If this is not possible, an attempt should be made to gain time for the best possible preparation, e.g. to develop therapeutic options and/or vaccines, to conduct studies on the properties of the pathogen, to increase treatment capacities in hospitals and to time the outbreak so that it does not coincide with other infection events (e.g. the annual 'flu wave').
Protection of vulnerable groups
Once it is no longer possible to prevent the spread of the pathogen, protection then focuses on individuals and groups with an elevated risk of severe disease.
Mitigation
If the disease becomes so widespread that the strategy of protecting particularly vulnerable groups is no longer possible, measures then focus on mitigating further negative impact on the public and on mitigating the impact on the life of society.
Situation-specific communication
Particularly at the beginning of a biological emergency, it must be assumed that it is not known what properties the pathogen possesses or even which pathogen it is. This uncertainty must also be communicated. It must be made clear which, what is being assumed and what further investigations are underway in connection with that.
One particular concern in communication on infectious diseases is the fact that members of the public suddenly see their neighbours/fellow human beings as a threat. It is therefore very important to provide information on routes of infection and protective measures. If a shortage of protective means is foreseeable, priorities will also need to be set. These must be weighed up very carefully and communicated clearly – if possible before a crisis arises. In 'quiet times' almost anyone will agree that in a medical crisis, medical personnel who take care of the sick must be given preference for prophylaxis.
Concerning risk communication and crisis communication please refer to the chapter ‘Communications’.
Alert system, notification channels
In Germany, pursuant to the Protection against Infection Act (IfSG) physicians, heads of facilities and laboratories are obliged to notify the responsible health office forthwith. The health offices are obliged to notify the supreme regional health authority, which in turn notifies the RKI. A prerequisite for this is 24/7 availability. Pursuant to Section 25 in conjunction with Section 16 of the IfSG, the health office shall without delay conduct investigations into the source of the pathogen and into patient contacts. It shall also define measures to prevent spread (prohibition of activities/visits, observation, isolation in the home, or e.g. isolation in an appropriate hospital pursuant to Section 30 (6) IfSG....).
A joint decision should be taken together with the treating facility, the press office and the supreme regional authority as to how and when the public shall be informed. To this end a press conference should be convened at short notice. Responsibilities will be defined beforehand: Who will leave the press conference, who will say what, and on which topics?
For further information on the alert system and notification procedures please refer to the sections 'Alert system' and 'Notification channels' in the chapter 'Operational planning'.
Management structure
The management structure for crises is described in detail in the chapter 'Operational planning'.
Actors and tasks
In biological emergencies primary responsibility rests with the health office, which must perform numerous tasks in this situation.
Examples include:
-
Risk assessment
-
Risk and crisis communication
-
Internal communication
-
Public information
-
Preparation of press work, possibly setting up of hotline
Contact tracing, definition of anti epidemic measures pursuant to IfSG, categorisation of contacts
Routine epidemiological surveillance -
Occupational safety and health, ensuring provision of personal protective equipment
-
Ordering of diagnostic measures and decision on scope of investigation
-
Protective measures to reduce contacts
Instructions on behavioural measures
Organisation and monitoring of patient
Regulation of sampling and transport of samples -
Information and advisory tasks for other authorities, facilities and the public
-
Definition and monitoring of isolation arrangements
-
Decision-making on nature and scope of disinfection measures and their monitoring, as well as expert advice
-
Possibly decision-making on decontamination measures
Ordering of isolation by the medical officer -
Ordering of autopsy, certification of death, oversight of transport of corpses and cremation
-
Disposal management
-
Possibly coordination of vaccinations
-
Possibly coordination of post-exposure prophylaxis
Documentation and evaluation
As well as the health offices, the regional authorities and health ministries are also involved when an incident occurs. Each federal state has its own specific rules governing precisely which tasks they perform in an emergency.
The RKI is a scientific-cum-medical institution of the German Government with a mandate for public health. It is responsible for fighting communicable diseases. The RKI plays a special role in further developing methods and designing scientific standards, e.g. for investigating suspected cases of the deliberate release of pathogens, which are referred to it as the designated body. In accordance with statutory provisions, the RKI advises primarily the professional public and policymakers. Nevertheless, it also sees its task as being to inform citizens and patients on infection risks and health trends, or refer them to other sources of information. In order to respond appropriately to a threatening situation or one perceived as such, and improve their own health situation, as many interested parties as possible should be able to form their own opinion. To facilitate this, in 2016 the RKI published further information in its brochure Protecting Health – Assessing Risks.
The Permanent Working Group of Competence and Treatment Centres (STAKOB) is another important actor in biological emergencies. STAKOB is a Germany-wide network of experts for the management and care of patients with high consequence infectious diseases. The competence centres possess special expertise in the field of public health, while the treatment centres specialise in the clinical care of patients with highly pathogenic, life-threatening diseases in special isolation units. STAKOB Can also be contacted for advice by telephone.
Other actors are the various health care providers. These include doctors' offices (outpatient care) and hospitals (inpatient care). Laboratories and pharmacies are also involved.
Finally, in an epidemic – and in a pandemic – all employers, together with the responsible company doctors, have these occupational safety and health tasks.
Particularly when a bioterrorist attack is suspected, other actors are also involved:
-
the police, to determine whether the suspicion is warranted. They will assess whether there is a serious threat. If they find that there is, further measures are necessary such as ruling out explosives. The police will then be responsible for cordoning off the crime scene and identifying the perpetrators.
-
the fire brigade in case of a biological emergency, in order to prevent the further spread of biological agents. The fire brigade will often assume responsibility for taking samples on behalf of the medical officer.
-
the Analytical Task Force (ATF) has been equipped with special measurement technology by the Federal Office for Civil Protection and Disaster Assistance. ATFs are stationed 10 locations in Germany. They can deploy anywhere they are called to within a maximum of three hours. If powder is found they are responders of choice for measurements to rule out the presence of chemical substances or radio-nuclear materials.
Resources
Staff
The key resource in biological emergencies is staff. Here there needs to be a focus on measures for occupational safety and health (personal protection measures).
In biological emergencies, a shortage of medical personnel trained in the use of personal protective equipment (PPE), including emergency service personnel, can arise very quickly. The shortage of trained staff is further exacerbated when the infection protection set is used, due the short time for which it can be worn and the physical strain it places on the individual wearing it.
Personal protective equipment (PPE)
In the event of a Germany wide-crisis,, PPE will very quickly be sold out. Accordingly, precautionary steps must be taken to stockpile sufficient quantities of PPE (BUT: Remember that PPE has a limited shelf life).
What constitutes a sufficient quantity is dependent on the risk assessment, what scenarios are to be expected and what dimensions they might assume within your sphere of responsibility. You also need to take into account the wearing times. As described in the 'Toolbox' chapter with respect to occupational safety and health, per suit the infection protection set is much cheaper than a suit with a blower unit. However, since the set can only be worn for a short time – a maximum of two hours, and for wearers who lack experience significantly less – consumption is much higher.
Packaging materials for samples
To be able to ship samples quickly and safely in a biological emergency, you should keep a sufficient stock of packaging materials (P620). Incorrect packaging material can also cause sample material to leak out of the package and thus contaminate people.
Furthermore, 'improvised' packages can be difficult for laboratory personnel to open, thus wasting valuable time.
Other resources
Other resources, such as medicines for PEP and therapy, isolation facilities, staff to monitor domestic quarantine, and hospital capacities – especially beds with ventilators and isolation beds – are covered in the 'Toolbox' chapter.
Outpatient care
Outpatient care plays a major role in Germany's influenza pandemic planning and its planning for COVID-19. The RKI's pandemic preparedness plan states
'To safeguard the needed resources for inpatient treatment in cases of severe disease, care should continue to be provided on an outpatient basis for as long as possible." (Structures and measures, national pandemic preparedness plan, RKI)
Concerning the management of suspected COVID-19 cases, the RKI states
'In certain situations in which inpatient admission is not necessary from a clinical point of view, if certain conditions are met (see table) this can be performed in outpatient care." (Notes on the outpatient management of suspected COVID-19cases, RKI, as at 27 February 2020).
The organisation and risk management of outpatient care should be planned before a crisis arises.
'Beyond the provision of basic services, responsibility for outpatient care lies with the associations of statutory health insurance physicians as part of the obligation to ensure care pursuant to Section 72 of Volume 5 of the German Social Insurance Code (SGB V)'. (Structures and measures, national pandemic preparedness plan part 1, RKI)
To ensure the quality of outpatient care it is urgently necessary to provide doctors in private practice with information materials geared specifically to their work. These should comprise practical handouts, e.g. on taking case histories, providing counselling, sampling, diagnostic laboratories, and protective measures for the doctor, their staff and other patients. The published recommendations of the German Medical Association and the Statutory Accident Insurance Association for Health and Welfare Services (BGW) include special instructions for risk management in medical practices.
Hospital allocation, inpatient care
When the number of persons injured exceeds the immediately available resources of the emergency services, the term 'mass-casualty incident' (MCI) is used. This textbook will provide more information on this, and on screening and hospital allocation, later on.
In Germany, which hospital allocation systems are used when the emergency services are working normally varies from region to region. In what biological emergencies the allocation systems seem appropriate for routine operation/MCI, or whether alternative allocation systems should be used, needs to be defined.
Ideally an allocation system will be interlinked not only with inpatient care, but also with the outpatient sector. It will then be possible to alleviate pressure on the inpatient sector when necessary.
Extensive preparations are also required in the inpatient sector. The RKI's pandemic preparedness plan states
'It is especially important to ensure that the admission and care of influenza patients are physically separate from general patient care, and that additional bed capacities are created, for instance by postponing elective operations.' (Structures and measures, national pandemic preparedness plan part 1, RKI)
Concerning the need for personal protective equipment (PPE), see the chapter 'Toolbox'. It is also important to consider the increased need e.g. for medicines.